ASLP Specialty Labs
We support community engagement activities like nonprofit professional development, service learning and volunteerism, community engaged research, social entrepreneurship and public-private partnerships.
We support community engagement activities like nonprofit professional development, service learning and volunteerism, community engaged research, social entrepreneurship and public-private partnerships.
Are you between the ages of 40 and 85 years old and suspect you have hearing loss? If so, you may be a candidate for a new study at the University of North Texas Speech and Hearing Center. To learn more about the "Impact of Listening Effort on Hearing Aid Adoption and Performance in Adults Ages 40-85 Years" and how you can qualify to participate, click here.
Current and future projects
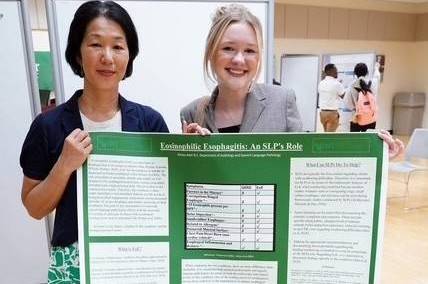
Some of the current projects include:
We are planning to study consonant sequences in other languages, including Spanish and French. Future projects are also planned for neural correlates of phonetic categorization in L2 speakers, and extending our work on typically-developing children to clinical population.
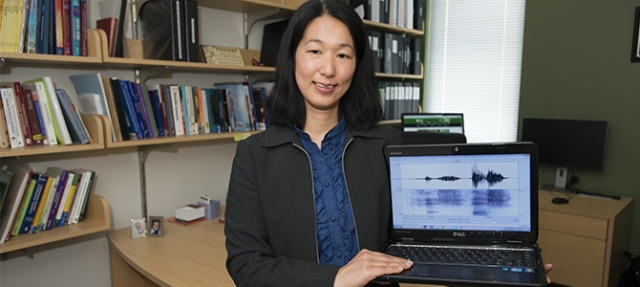
Dr. Aoyama’s current vita is on UNT’s Faculty Information System.
She also has a profile on Google Scholar and on Research Gate. Her ORCID is 0000-0002-3534-8811.
Please contact kat.aoyama@unt.edu for further information.


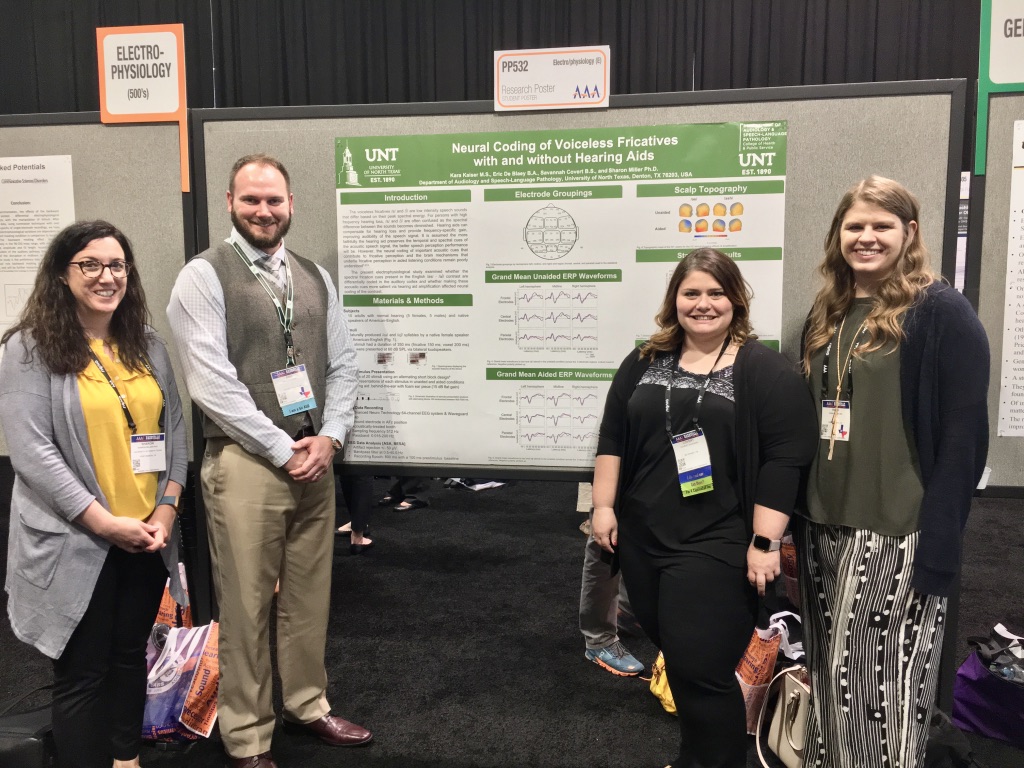
Current projects
Publications
¥ Denotes mentored student author. The first last name of author list is the ‘first author.’ Miller, S.E.* denotes that I was the corresponding author.
Lab Members:
Director: Dr. Boji Pak-Wing Lam
Boji Lam is an assistant professor in the Department of Audiology and Speech-Language
Pathology. His research adopts a multidisciplinary approach to examine the effect
of bilingualism and motivation on language behaviors, learning, and therapeutic outcomes
in both children and adults.
Our Research
Publications:
We are currently recruiting participants for a study on executive function. Please refer to the flyer for more details and email us
at blam.study@gmail.com.
Location: ASLP Room 268
Peterson has a type of aphasia similar to what we call Wernicke’s aphasia and is talking about his vacation activities
Researchers and rehabilitation specialists worldwide are working together to design ever-more-effective medical and behavioral interventions for people with aphasia, based on principles of rehabilitative neuroplasticity. Often, aphasia persists even after the person with aphasia has been discharged from the hospital, and they may live with aphasia for a lifetime. For this reason, multi-disciplinary groups of researchers and advocacy organizations around the globe (such as Aphasia Access: https://www.aphasiaaccess.org/) conduct research and engage in social action designed to reduce and remove the medical, economic, psycho-social, and social barriers to long-term health and quality of life for people with aphasia, and to open doorways to their participation in everyday life contexts of their community.
Dr. Olness’ lines of NIH-funded discourse research examine the discourse production abilities of adults with aphasia, with a focus on narratives, including personal stories from everyday life. In 2018, the anonymized data collected on this project were contributed to Aphasia Bank (an NIH-funded, shared repository of clinical-discourse-research data sets), in support of advancement of global aphasia research, with the informed consent of the approximately 80 narrators with and without aphasia from a large urban area in the southern United States who participated in the project. Patterns of normal discourse variation, such as ethnic discourse styles of African Americans and Euro-Americans, formality, spontaneity, and age/cohort effects, are incorporated into Dr. Olness’ approach to analysis. Dr. Olness’ basic-research interests focus on the relationship between linguistic and paralinguistic forms and how they operate together as communicative tools for people who have aphasia: How might residual language abilities, prosody, gesture and other channels of communication operate together, so the person with aphasia can communicate about events in their life and express their stance (emotion, opinion, and attitude) about those events, despite their aphasia? When and where might their aphasia get in the way of successful personal narration? As humans, the ability to share personal stories from our lives allows us to express our identity and personal opinions to others, bonds us with other people, and helps us to “make sense” of the events in our lives. How does aphasia impact a person’s ability to “tell his or her story”? And to maintain and express his or her identity?
From a basic-science perspective, discourse research with populations who have aphasia also sheds light on the cognitive-linguistic and neurological substrates of “normal” discourse production and communicative functionality of non-brain-injured populations. The Aphasia Bank data also contribute to these global lines of research.
It is important to bridge basic research to clinical research and evidence-based clinical practice. Dr. Olness’ combined areas of inquiry are applied to the design of clinical discourse assessment and the design of intervention to augment functional communication of people with aphasia in their everyday life contexts. The UNT research team led by Dr. Olness has been collecting and analyzing anonymized data with the informed consent of a group of research participants with aphasia engaged in group conversation, with a specific focus on how people with aphasia embed personal stories into these conversations, and their degree of success in incorporating stories from their life into the flow of the conversation. These pilot data are guiding the team in the development of a valid, reliable, and clinically feasible assessment tool, so clinicians can gauge the communicative functionality of people with aphasia and their conversationalists, as they weave personal stories into conversation. These lines of research are further supported through the newly founded Scientific Collaboration on Interactional Discourse and Communicative Diversity (SciCID-CD), a seven-institution, national collaboration of researchers co-convened by Dr. Olness and Dr. Julie Hengst (University of Illinois) and launched in Fall 2019.
Also in Fall 2019, Olness and collaborators in UNT Engineering (Drs. Ifana Mahbub, Diana Berman, Mark Albert, and Ting Xiao) launched a collaborative project designed to contribute to clinical intervention for people with aphasia (Wireless Smart Vocalization Sensors for Convergent Evidence of Rehabilitation Effectiveness). The long-term goal of this project is to develop a wearable, wireless, and user-friendly engineered system that provides objective, continuous, real-time feedback to both the user with aphasia and the clinician, regarding the user’s communicative engagement as they go about their daily routine, while still maintaining confidentiality of the user’s communicative content.
For the past several years, and with funding support in 2018 from the Southwestern Medical Foundation, Josephine Simonson Aphasia Trust Fund, Dr. Olness and a multi-disciplinary, multi-institutional collaborative team of researchers, clinicians, and people with aphasia have been conducting lines of research on the medical, economic, social, and geo-spatial landscape of barriers and facilitators that North Texans with aphasia navigate, toward long-term health, quality of life, and participation in everyday life contexts of the community. Using estimates of aphasia incidence and prevalence, surveys of public awareness of aphasia, and assessments of availability of and access to post-discharge supports and services for people with aphasia and their families, we are starting to map the landscape of barriers and facilitators to communicative access and life-participation for people impacted by aphasia in our community.
Prior to joining the UNT ASLP faculty in 2006, Dr. Olness worked as a federally funded (NIH) Research Scientist at the University of Texas at Dallas (UTD) Callier Center. Dr. Olness received her doctoral and post-doctoral training at UTD (formerly School of Human Development and Communication Sciences, and currently School of Behavioral and Brain Sciences), under the mentorship of Dr. Hanna Ulatowska. Earlier degrees were in Linguistics (M.A., U. of Oregon), and Communicative Disorders (M.S., U. of Wisconsin--Madison). She began her career as a B.A. double major in French and Speech & Hearing Sciences (Indiana U., - Bloomington) under the mentorship of Dr. Judith Johnston.
Publications authored and co-authored by Olness have appeared in Aphasiology, Brain and Language, Discourse Processes, the Journal of Neurolinguistics, the Journal of Speech and Hearing Research, and Advances in Speech-Language Pathology, inter alia. She has been invited by the organizers of the annual meeting of the Science of Aphasia (Italy), Hadassah Academic College and Adler Aphasia Center (Israel) and the Aphasia Institute (Canada) to deliver addresses and keynote presentations to global audiences on her lines of basic and applied research.
Olness’ clinical training in adult neurogenic communication disorders includes a graduate internship at the Middleton V.A. Hospital (Madison, WI) under Dr. John (Jay) Rosenbek, and a Clinical Fellowship at Northwestern’s Rehabilitation Institute of Chicago (RIC; currently renamed as the Shirley Ryan Ability Lab). She continued her clinical work as a staff speech-language pathologist in a non-profit clinic in Eugene, Oregon. Her current clinical research program involves on-going contact with and advocacy for individuals who have aphasia.

 Get Involved:
Get Involved:
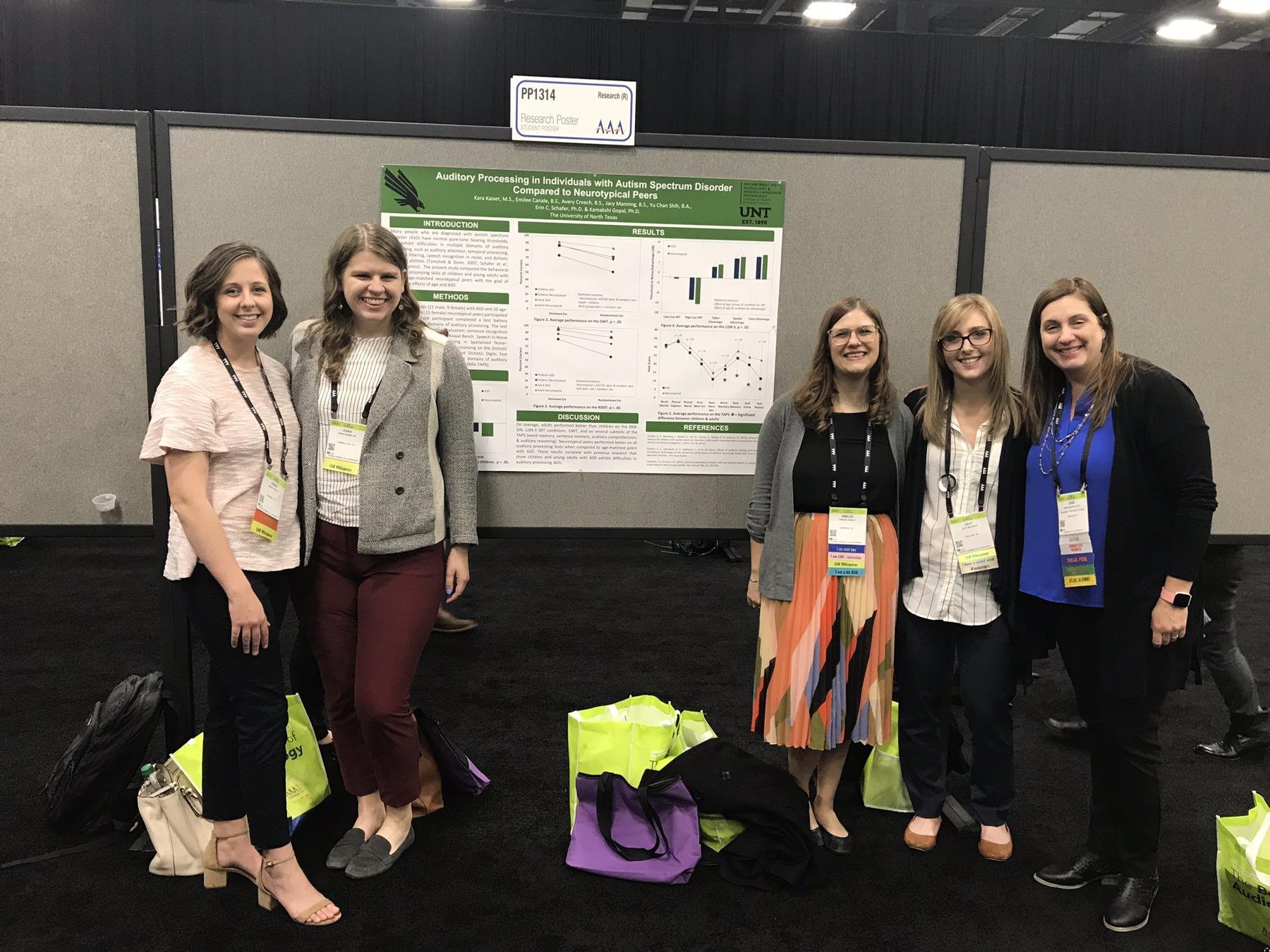
If you are a UNT student and are interested in working or volunteering in the lab,
please contact Erin.Schafer@unt.edu.

An additional area of research that Dr. Gopal engages in is the prevention of recreational hearing loss.
Dr. Gopal’s multi-disciplinary research team consists of UNT faculty members in the departments of Behavioral Analysis, Biological Sciences, Audiology and Speech-Language Pathology, Advertising, Engineering, and Music as well as external members, including the Director of the WHO Division of Prevention of Hearing Loss, UTSW Medical Center - Department of Radiology, and UNT HSC – Department of Population & Community Health.
During her tenure at UNT, Dr. Gopal has received over 1.4 million dollars in intramural and extramural grant money and has had numerous publications and conference presentations.
Dr. Gopal’s current research interest is in identifying the relationship between hearing and cognition, as well as how hearing aids can prevent or delay cognitive decline.
The Department of Audiology and Speech-Language Pathology strives to provide the finest professional education in both speech-language pathology and audiology while maintaining an excellent Arts and Sciences pre-professional undergraduate degree.
The Center offers state-of-the-art diagnosis and treatment of speech, language, and hearing disorders.